In 2022, a global consulting firm projected that the United States would face a shortage of 200,000 to 450,000 registered nurses (RNs) for direct patient care by 2025. According to federal data cited by the American Hospital Association, around half a million nurses were expected to leave the profession by the end of that year, resulting in a total shortage of 1.1 million. These figures are not errors or mere statistics; they represent a significant imbalance where the demand for bedside nurses will surpass the supply, affecting health systems nationwide.
Nurses are vital members of the patient care team and the cornerstone of the healthcare sector. However, the nursing profession has been grappling with shortages for decades. The extent of these shortages varies by study and state, but regardless of the perspective, the issue poses a critical challenge to the nation’s healthcare infrastructure. Current data indicates that while some states may face a severe shortage, others might actually experience a surplus of nurses.
What Are the Causes of Nursing Shortages?
The ongoing nursing shortage is a complex crisis driven by both deep-seated systemic challenges and pressing current issues. At the heart of the problem is the aging population, which increases the demand for healthcare services, while the nursing workforce itself is aging, resulting in a significant wave of retirements.
Simultaneously, a persistent bottleneck in nursing education, caused by faculty shortages, restricts the number of new nurses entering the field. Additionally, heightened stress and burnout, worsened by the COVID-19 pandemic, have led to a considerable number of experienced nurses leaving the profession.
10 Factors Leading to Nurse Shortages
Each of the following factors adds to the complexity of the nurse staffing challenge:
- Aging Population: The large baby boomer generation is aging, and by 2030, all will be 65 or older. This increases the demand for complex care and more nurses.
- Aging Workforce: The nursing workforce is also aging, with about one million RNs expected to retire between 2017 and 2030. This will significantly reduce the number of experienced nurses.
- Increased Burnout: High-stress environments, long hours, and emotional demands are causing unprecedented levels of burnout among nurses, leading to decreased job satisfaction, increased absenteeism, and many nurses leaving the profession.
- Nurses Leaving Bedside Jobs: More nurses are leaving high-stress bedside roles for other positions in healthcare or different industries. Reasons include burnout, unsafe staffing ratios, inadequate support, low pay, lack of appreciation, insufficient breaks, and inadequate mental health resources. As of February 2023, nursing turnover rates ranged from 8.8% to 37%, depending on specialty and location.
- Faculty Shortage: In 2021, nursing schools turned away nearly 92,000 qualified applicants due to capacity issues like insufficient clinical sites, classroom space, faculty, and clinical preceptors. Low salaries for faculty roles make these positions less attractive.
- Affordable Care Act (ACA) Impact: The ACA’s healthcare expansion increased demand for services, adding pressure on the nursing workforce.
- Growing Interest in Community-Based Care: The shift towards community-based care models requires more nurses outside traditional hospital settings, stretching the workforce further.
- Economic Incentives in Other Fields: Competitive wages and less stressful working conditions in other sectors attract trained nurses away from nursing careers and reduce the number of new entrants into nursing programs.
- Violence in Healthcare Settings: Emotional or physical abuse in healthcare settings adds to the stress, with healthcare workers being five times more likely to sustain injuries from workplace violence than those in other professions.
- Physician Shortage: The Association of American Medical Colleges (AAMC) predicts a shortage of 37,800 to 124,000 physicians by 2034, including 17,000 to 48,000 in primary care. This increases the workload for nursing staff and the demand for advanced practice nurses.
Impact of the Ongoing Nurse Shortage on Employers
Why is the nursing shortage such a concern? A lack of nurses often leads to understaffing, which can compromise patient care quality. This, in turn, affects outcomes, patient satisfaction, and facility revenue. Understaffing also increases workloads, burnout, and turnover, and can lead to nursing strikes, driving up costs for overtime and temporary workers. Additionally, it worsens the nursing shortage by contributing to more nurses burning out and retiring early.
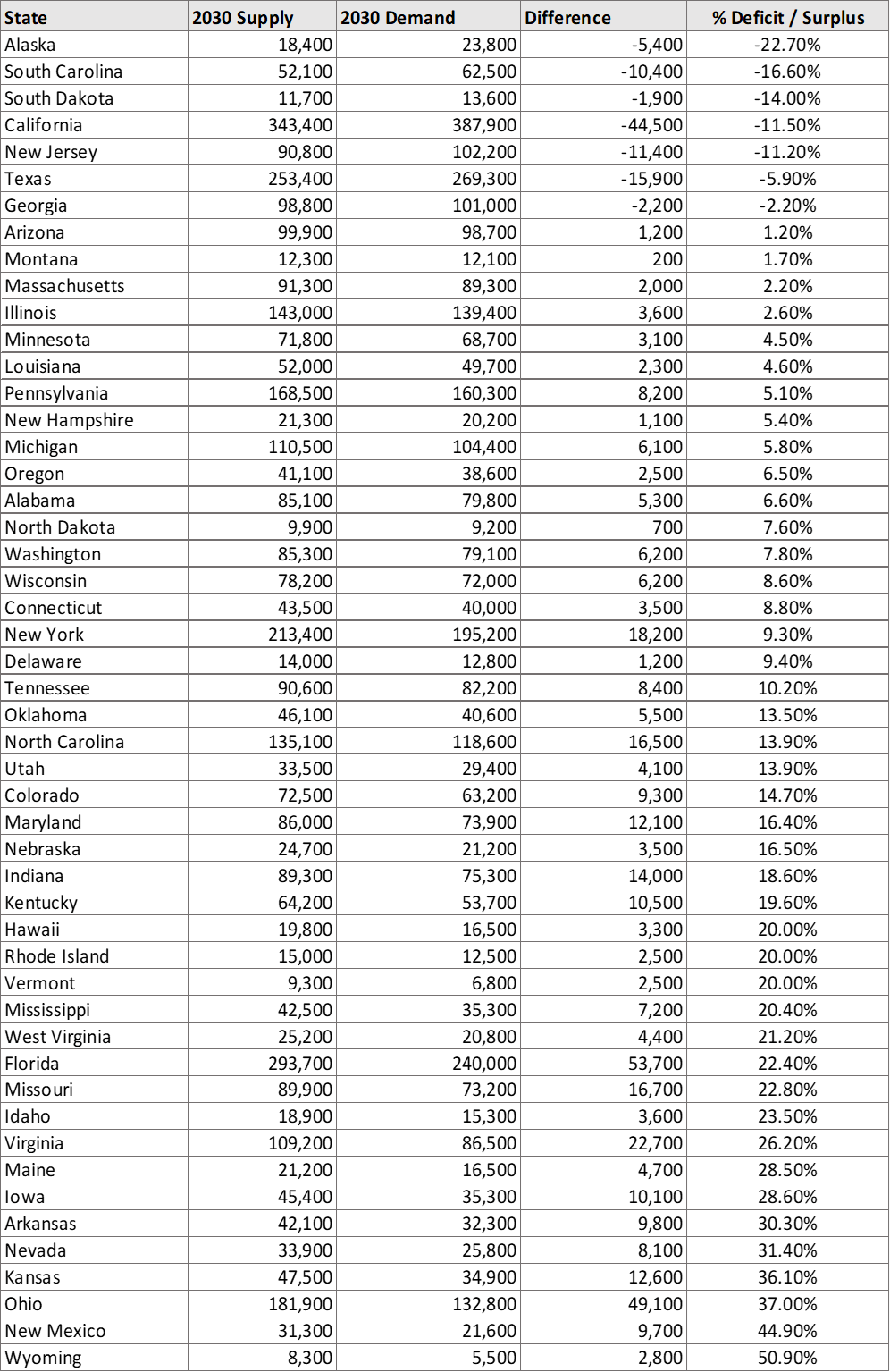
Expected RN Deficits Across States Until 2030
Analyzing the national nurse shortage by state reveals that some states may lack sufficient nurses and have limited growth prospects, while others may have more nurses than needed. Unfortunately, recent state-by-state reports rely on data collected before the COVID-19 pandemic, which had a significant impact on healthcare professionals. These reports also do not include nurses who left the profession during or shortly after this crisis.
In this update, we used projections from the Health Resources and Services Administration’s (HRSA) Bureau of Health Workforce (BHW). They evaluated each state’s projected RN supply and compared it to demand for 2030 to identify state-level shortages and surpluses. The following table ranks states from the largest expected shortage to the largest surplus.
It’s important to note that these projections are somewhat outdated. While the table suggests only seven states are projected to face shortages based on this report, preliminary data in the upcoming version indicates several more states may experience shortages. Additionally, state-by-state projections for registered nursing shortages vary across different sources, so one report might show your state with a surplus while another predicts a shortage.
Projected Need for Registered Nurses
To understand how the COVID-19 pandemic may have affected the shortage or surplus projections mentioned in HRSA’s report, let’s examine its impact on nurse availability from 2020 to 2022. According to research by the National Council of State Boards of Nursing (NCSBN), approximately 100,000 RNs exited the workforce nationwide during these two years of the pandemic. To assess this impact at the state level, we compared the number of employed RNs in 2020 with those in 2022 to identify states where the nursing workforce decreased instead of increasing as expected.

Certain states may experience equilibrium between supply and demand
Despite uncertainties about nationwide RN shortages or surpluses, some states are beginning to observe a balance in supply and demand.
For instance, California, which was projected to have an 11.5% deficit by 2030 according to the HRSA report, reported a projected gap of 6.2% by the end of 2022 in its own 2022 Forecasts of the Registered Nurse Workforce in California report by the University of California, San Francisco, and supported by the California Board of Registered Nursing. The report predicts that RN shortages will continue until 2029 when supply and demand are expected to stabilize, leading to a surplus of 8.1% by 2037.
On the other hand, Alaska continues to face challenges in its nursing workforce. While it had the highest RN deficit in the HRSA’s 2014-2030 report at 22.7%, it did not rank among the top 10 states in the upcoming 2020-2035 projections.
According to the Alaska Healthcare Workforce Analysis published in December 2022, RNs are the most needed healthcare professionals annually in the state to meet growing demands. In 2021, Alaska had 6,995 RNs with an average turnover rate of 21%. The state requires 1,463 new nurses for replacements and 81 more for growth, totaling 1,544 new RNs needed each year.
Alaska has historically struggled to attract and retain skilled nurses and other medical professionals, worsened by the pandemic. For nurses seeking job stability, Alaska offers opportunities. In addition to RNs, LPNs are also projected to experience a shortage of 36%.
The 2022 Alaska Hospital and Healthcare Association Salary and Benefits Report indicated that hospital RN vacancy rates averaged 24% in 2022, with an average of 161 days to fill vacant positions. Travel nursing roles in Alaska are often plentiful and offer above-average salaries, helping to address staffing shortages in hospitals, nursing homes, and assisted living facilities.
Is the Nursing Shortage Real?
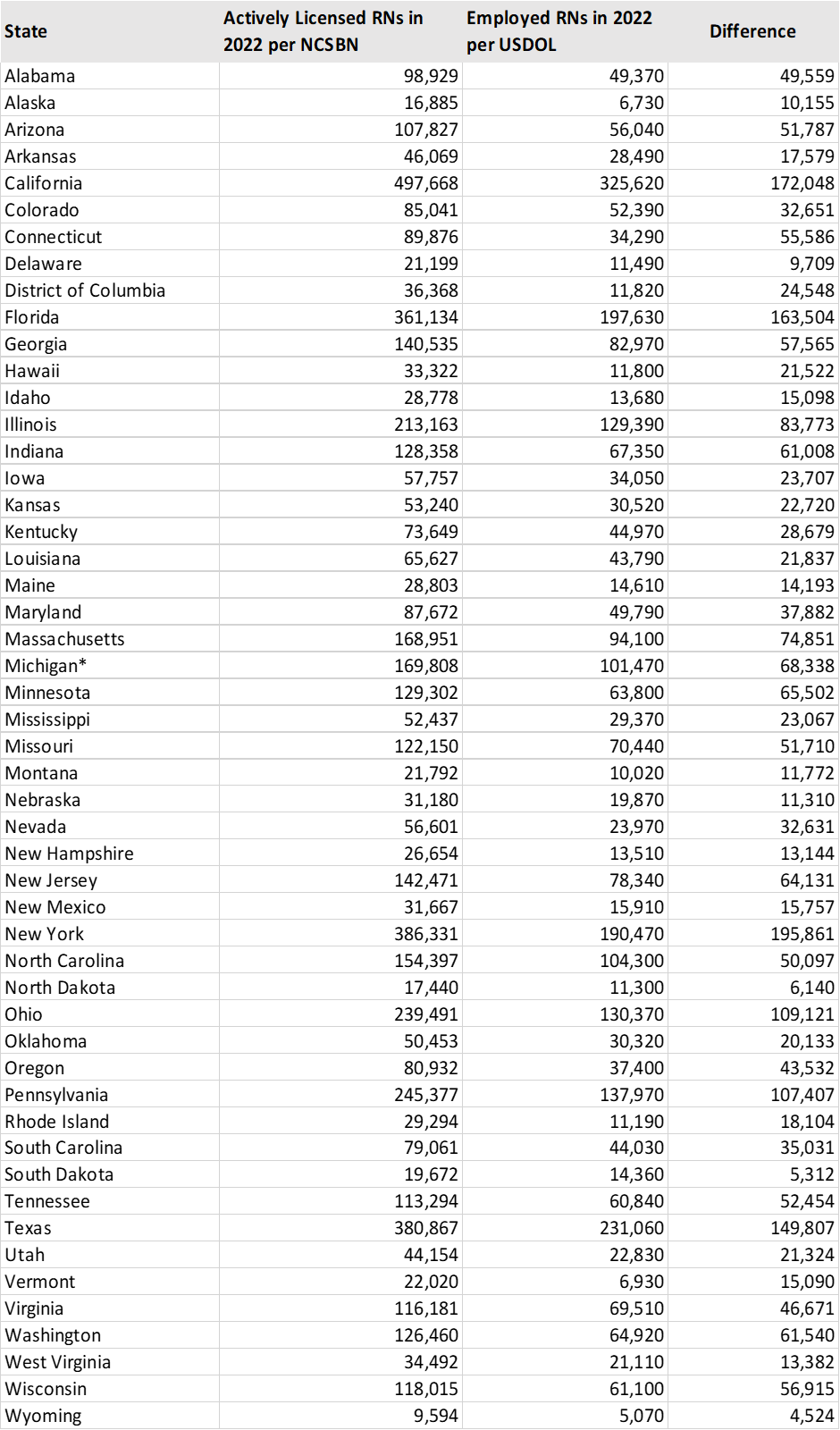
Some organizations and nursing unions argue that while there are plenty of registered nurses with licenses, not enough of them are actively working in the field. Despite reports of recurring shortages of RNs over many years, there is no definitive measure to confirm the existence of a labor shortage, although many RNs report experiencing frequent staffing shortages in their workplaces.
Although increasing RN vacancy rates indicate a potential shortage, higher vacancies may be temporary, such as during severe flu seasons, seasonal fluctuations, or when new hospitals are built. Health systems may also list job vacancies without actively seeking to fill these positions.
In 2020, Oregon had 59,778 licensed RNs, but only about 75% were actively practicing, according to the Oregon Hospital Association. Similar patterns were seen in other nursing roles, with approximately 86% of CNAs, 83% of LPNs, and 78% of APRNs actively practicing compared to the number licensed during this period.
As of the end of 2022, the NCSBN reported over 5.3 million active RN licenses nationwide. However, holding a license does not necessarily mean that all these professionals are actively working in bedside nursing. Some may be retired, hold multiple single-state licenses for travel nursing, or use their nursing credentials in roles such as teaching, consulting, or writing, which do not involve direct patient care.
The RN shortage could be worse if we exclude those with active licenses who aren’t practicing. Below, we compare the number of actively licensed nurses by state based on 2022 NCSBN records with employed RNs based on 2022 USDOL records.
What About Nurses in Other Roles?
According to the BLS, in 2022, 59% of RNs worked in hospitals, whereas only 15% of LPN/LVNs did. Nearly half of licensed practical/vocational nurses worked in nursing and residential care facilities or home healthcare services during this time.
While most attention focuses on shortages of registered nurses, the HRSA’s 2022 Nurse Workforce Projections also anticipate growing demand for LPN/LVNs. The report projects a national shortage of 141,580 LPN/LVNs by 2035, with demand outpacing projected supply between 2020 and 2035, resulting in an overall shortage of 17% compared to a 5% shortage in 2025.
Similar to RNs, the shortage or surplus of LPN/LVNs varies by state. According to the HRSA, Alaska faces the most significant challenge with an 88% shortage of LPNs, while Arkansas anticipates a surplus of 51% by 2035. Additionally, NCSBN research indicates that LPN/LVNs have seen a decline of 33,811 since the start of the pandemic, and this downward trend continues.